Autism Spectrum Disorder (ASD): An All-in-One Guide
The term autism is not what it once was. “Autism” originally described a severe set of schizophrenia symptoms in 1911 by a German psychiatrist named Eugen Bleuler. This misconception continued until the 1960s when child psychology became a science.
Autism Spectrum Disorder Guide:
- Some common myths about ASD include:
- Recognizing the Early Signs of Autism Spectrum Disorder
- Early Signs Of Autism
- Developmental Regression
- Diagnosing ASD
- The Causes Of Autism
- Autism Heredity
- ASD and Hyperemesis Gravidarum
- Autism Therapy and Tools
- Floortime Play Therapy
- IEP Goals for Autism
- Video Modeling and Autism
- Autism and Speech
- ASD and Speech Delay
- Nonverbal Autism
- PECS And Autism
- How To Customize PECS For Your Child
- Stimming Behavior
- Oral Stimming
- Sensory Issues
- Synesthesia and Autism
- Food Aversions and Autism
- Resources, Books and Magazines on Autism for Parents
Today, the term autism is now known as Autism Spectrum Disorder (ASD). It’s used to describe a complex developmental disorder affecting communication and social skills first appearing in childhood. When speaking about ASD, it’s important to separate myths from facts about the developmental disorder.
Welcome to our series of “All-in-One” guides connecting blog writers around an important topic that is explored in-depth on our blog page. The subject of this guide explores what parents need to know about Autism Spectrum Disorder (ASD). You can download the whole guide as an ebook here:
Some common myths about ASD include:
Autism is curable.
- Fact: Autism is not curable. It’s a lifelong developmental disorder.
Individuals with autism cannot live an independent and successful life.
- Fact: People with autism can live full, happy, and successful lives with the help of speech and occupational therapy.
The cause of autism is bad parenting.
- Fact: There is no known single cause to autism. Studies suggest the development of autism occurs before birth.
Individuals with autism do not speak.
- Fact: Autism is complex. Some people develop speech normally, while others communicate with a combination of words, gestures, and communicative devices.
These common misconceptions about autism only show the need for awareness. That’s why April is Autism Awareness Month. To better understand this developmental disorder, parents need to know how to recognize the disorder affecting 1 out of 110 children.
Recommended article
Autism Awareness Month: Spreading the Word
Recognizing the Early Signs of Autism Spectrum Disorder
Autism is a complex disorder in which no two children or adults display the same signs and symptoms. It is also a disorder affecting different areas of a person’s life. While one area may be greatly affected, another area may exhibit no signs of autism. For example: A child may struggle with sensory issues, but is able to talk in back and forth communication.
Early Signs Of Autism
Social
- Cannot self-regulate emotions
- Trouble adjusting to a new environment
- Can only focus on one task at a time
- Does not respond to questions correctly or respond at all
- Cannot communicate in back and forth conversation
- Trouble relating to others
Language
- Loss of language previously acquired around the age of three
- First words are nouns (objects) instead of proper nouns (names) and verbs (actions)
- Noncommunicative gestures and expressions are delayed the first year (waving goodbye or pointing)
- Repeats words immediately after being heard. Also known as ‘echolalia.’ Delayed echolalia also occurs in which a child repeats words heard for hours, days, or weeks.
- Limited eye contact with others
- Speech may be robotic and words may not flow together
- Does not understand social norms of communication like the volume of voice or speaking over someone
- Trouble understanding humor or sarcasm
- Craves structure and predictability
- Little to no fear
- Unable to plan or organize tasks
- Poor problem-solving skills
- Does not use toys appropriately or for their intended purpose
- Repetitive play
Behavior and Emotional Regulation
- Cannot handle changes in routine
- Trouble applying learned skills
- Uses objects differently or develops an attachment to certain objects or toys
- Stimming behavior (rocking, chewing, hand flapping)
- Unusual ways of expressing emotions (aggressive behavior, meltdowns, tantrums, running away)
- Repetitive and strict patterns of play, interests, and behavior
- Cannot self-manage well
Sensory and Eating
- Overreacts or under reacts to environmental stimuli like light, sounds, and social situations
- Plays by themselves
- Particular about food choices because of sensory issues
- Prefers a limited amount of food choices
Recommended article
Signs of Autism Spectrum Disorder
Developmental Regression
Developmental regression occurs when a child loses an acquired skill. A potty-trained toddler starts having accidents again. A talkative child reverts to babbling or using nonsense words. For many children, a developmental regression is only temporary and may be the result of mastering a new skill or a major life change.
Developmental regression occurs when a child loses an acquired skill.
But for some children, they are experiencing a regression due to the onset of autism symptoms. For the first year, many children who are later diagnosed with autism develop normally. It is possible for a child under one to show no signs of autism. However, once the child reaches the age of two, many parents notice autism signs that the child had not displayed before.
If a child experiences a developmental regression not related to mastering a new milestone or a major life change, an evaluation or screening for autism needs to be conducted.
Recommended article
Developmental Regression in Toddlers – What Can I Do?
Diagnosing ASD
Once a child displays signs of autism or a developmental regression, an evaluation for Autism Spectrum Disorder (ASD) should be conducted. Some children are diagnosed with autism as early as 18 months. For most children, a diagnosis of autism occurs after the age of two years old.
Although every child should be screened for autism at 9, 18, and 24 or 30 months by a pediatrician, signs of autism can still be missed. Some children with a higher risk of developmental disorders may need to attend additional appointments for further screening.
The diagnosis process for autism is a three-step process.
Step 1: Screening
Before a child is diagnosed, he or she must undergo an initial screening. This process takes roughly 15 minutes and involves a discussion and observation of a child’s acquired and delayed milestones and skills. For a child, this initial screening is stress-free. All a child has to do is play. The doctor will observe and engage with the child in play to see how the child speaks, learns, and behaves.

Step 2: Developmental Pediatrician
If the doctor from the initial screening feels further evaluations need to be done, the doctor will refer the child to a developmental pediatrician. A developmental pediatrician is a doctor specializing in childhood development. They can identify a multitude of behavioral and developmental disorders in children.
Developmental pediatricians are also able to help:
- Advocate for school planning and services needed
- Prescribe medications
- Initiate medical evaluations
- Provide long-term monitoring for a child’s development in educational programs and behavior management

Step 3: Full Comprehensive Evaluation
After a child is seen by a developmental pediatrician, a full comprehensive evaluation is conducted. A comprehensive evaluation is a more thorough process involving a child neurologist, a speech and language pathologist, and a child psychologist. All these professionals combined will help determine if a child has autism.
To determine if a child displays signs of autism or not, four tests are used to diagnose ASD:
- Autism Diagnosis Interview – Assesses a child or adult in three main areas of behavior (social interaction, communication/language, and restricted and repetitive interests and behaviors.
- Autism Diagnostic Observation Schedule – Examines social interaction, play, communication, and how imaginative a child is with materials.
- Childhood Autism Rating Scale (CARS) – Only used for children over the age of two years old and takes an in-depth look into behavior, abilities, and the characteristics of a child.
- Gilliam Autism Rating Scale – Suitable for diagnosis in children over three years old and tells parents, teachers, and clinicians the severity of the disorder.
Recommended article
How is Autism Spectrum Disorder Diagnosed?
The Causes Of Autism
Although there are many myths about the causes of autism, there is not one single factor known to cause autism. Instead, science is finding that autism is caused by a variety of factors.
So far, there are seven factors attributed to a child developing autism.
1. Role of Genetics
Each family unit stands a likelihood of 1 in 68, or has a 1.5% chance of having a child with autism. But since family members have a similar genetic makeup, families who have one child with autism are at a 20% greater risk of having another child with autism. The risk then increases to 30% if a family already has two or more children with autism.
Swedish researchers found connections between a family’s history of mental and neurological disorders like ADHD, schizophrenia, or depression, and the odds of having a child with autism. The results concluded:
- Children with a parent or sibling with mental and neurological disorders had 4.7 times greater risk
- Children with a family with mental and neurological disorders stood a 7.6 times greater risk of developing autism and intellectual disability.
Other studies yield similar results as well, contributing an increase in autism if a sibling has attention-deficit hyperactivity (ADHD) or a parent has depression, anxiety, bipolar disorder, or schizophrenia.
2. Birth Complications
The American Journal of Perinatology found children were at an increased risk for developing autism if they experienced birth complications. The birth complications found with the highest connection to autism include:
- Preeclampsia
- Placenta separation from the uterus
- Breech or transverse birth
- Oxygen deprivation during labor (birth asphyxia)
- Prolapse or exposed umbilical cord
While not one single birth complication pinpoints if a child will have autism or not, children who experienced the above complications do have an increased risk of developing autism according to research.
3. Genetic Disorders
Although it is rare, genetics may play a large factor in the risk and development of autism. Both Rett Syndrome and Fragile X Syndrome have been found to place a child at a higher risk of developing autism.
However, it should be noted that both disorders are extremely rare and are the result of genetic mutations.
4. Born to Older Parents
Some research studies from Denmark, Israel, Sweden, and California have found men over 40 years old are at a six-fold increase of having a child with autism. It’s suspected by researchers that men who have children over 40 years old may carry autism traits leading to delays in romantic partnerships and having children.
Other studies found different results that could debunk this theory. While being born to older parents cannot be eliminated as a cause of autism, it is still considered a theory with no concrete research to support it.
5. Low Birth Weight
Low birth weight is anything below 5.5 pounds. When a child is born with low weight and/or prematurely, they may be missing proper fetal growth to help them develop. The Center for Disease Control found children born less than 5.5 pounds had a 2.3-fold risk of autism. The same study also found girls born underweight had a 3-fold greater risk of autism.
6. Environmental Toxin Exposure
Heavy metals and environmental toxins are thought to be one of the contributing factors for causing autism. But this is simply a theory. As of today, there is no significant research to back up the theory.
The Children’s Environmental Health Center lists 10 common toxins and chemicals suspected of causing autism. Therefore, pregnant women should limit their exposure to the following 10 environmental toxins:
- Perfluorinated compounds
- Endocrine disruptors
- Methylmercury
- Lead
- Organophosphate pesticides
- PCB’s
- Organochlorine pesticides
- Brominated flame retardants
- Lead
- Automotive exhaust
7. Viral Infections
According to research from the American Society for Microbiology, pregnant women with active infections doubled their risk of having a child with autism. More specifically, certain viral infections have been found by research to be linked to the development of autism.
These six viral infections at the time of pregnancy double a woman’s chance of having a child with autism:
- Cytomegalovirus
- Measles
- Epstein-Barr Virus
- Rubella
- Human Herpes Virus 6
- Herpes Simplex Virus 1 and 2
Science is pointing to a mix of biology and environmental factors in combination that contribute to the development of autism. Not just one single factor. With increased research into the causes, it’s about finding a specific or “right” combination of different factors that directly influences autism development.
Autism Heredity
Since we know the role of genetics can play a part in the cause of autism debate, it’s important to discuss some common characteristics of heredity and an autism diagnosis.
- Those with a family member with autism are more likely to be diagnosed as well
- Boys are diagnosed with autism more than girls
- Vaccinated versus nonvaccinated children are equally at risk of an autism diagnosis
- Children with older parents tend to be at an increased risk of autism
- Premature babies born before 26 weeks show a greater risk of autism
While there’s no specific cause to autism, many professionals in the field of treating and diagnosing autism believe genetics and environment combined play a role. It’s believed other genes may affect a child’s brain development or how the brain cells communicate. It could also be that specific genes determine how mild or severe autism symptoms will be.
Although these are simply theories up for debate, the role of genetics, heredity, and environment are all key factors in determining the possible cause of autism.
For more on the role of heredity, read the article Autism… Is It Hereditary?
Recommended article
Is Autism Hereditary? Speech Therapist's Experience
ASD and Hyperemesis Gravidarum
Along with examining genetics and environment, the debate about hyperemesis gravidarum and autism needs to also be looked at as a possible cause. Hyperemesis gravidarum is better known as severe morning sickness. It’s categorized by excessive vomiting and nausea. The cause of severe morning sickness is thought to be hormonal changes and high levels of hCG (human chorionic gonadotropin hormone) during early pregnancy.
Although the exact cause of hyperemesis gravidarum is still unknown, symptoms tend to appear between 4 to 6 weeks. Many pregnant women find relief from symptoms around 14 to 20 weeks. But 20% of women still require care for severe morning sickness for the rest of their pregnancy.

Hyperemesis gravidarum is better known as severe morning sickness. It’s categorized by excessive vomiting and nausea.
Southern California Research and Evaluation Center found in a recent study that pregnant women with hyperemesis gravidarum were 53% more likely to have a child diagnosed with autism spectrum disorder. The study further found:
- Mothers with hyperemesis gravidarum diagnosed in the first and second trimesters put them at an increased risk of having a child with autism. But no increased risk for mothers who were diagnosed in the third trimester
- The severity of hyperemesis gravidarum did not increase the risk of autism
- Hyperemesis gravidarum and autism was higher among girls than boys and more prevalent in Caucasian and Hispanics than Pacific Islanders and African Americans
- Medications for treating hyperemesis gravidarum were not related to developing autism
Another study in 2018 conducted by Telethon Kids Institute found pregnant women with hCG levels that were too high or too low raised their risk of having a child with autism.
While both studies found a link between the risk of autism and hyperemesis gravidarum, it doesn’t mean severe morning sickness is the cause of autism. More research needs to be done to find or rule out the cause of autism including the severity of morning sickness during pregnancy.
Autism Therapy and Tools
After your child receives a diagnosis of ASD, it is overwhelming to think about doctor’s appointments, therapies, and changes at home. But the best part about autism therapy is it is not a “one size fits all.” Every therapy doesn’t work for every child. Therefore, all the different types of therapies are customized to meet your child’s needs. When treating children with autism, there are three therapies typically used.
1. Applied Behavior Analysis
This type of therapy is best suited for children who have been diagnosed with autism under the age of five. Applied behavior analysis is considered the “gold standard” for treating autism because it changes bad behaviors and reinforces good ones with a reward and consequences system. A therapist may want to observe and treat the child in a daycare, home, or playground where challenging behavior typically occurs.

While a “natural setting” is used for changing behaviors like meltdowns and tantrums, it’s also used for reinforcing or teaching imaginative skills or empathy through reward. This therapy is great for addressing challenging behavior but is an intensive therapy often requiring 20-40 hours per week.
2. Relationship Development Intervention
This therapy focuses on critical thinking, communication skills, and social interactions with the people closest to the child. Instead of the therapy focusing solely on the child, RDI includes the involvement of those closest to a child (parents and teachers).
Parent involvement is key with this therapy! You become your child’s therapist. Although it’s a new therapy, RDI yields promising results. To see success in your child with RDI, you need to be in regular contact with a program consultant and receive extensive therapy information that includes watching instructional videos and conferences.

Relationship Development Intervention has six objections:
- Emotional Referencing: Learning from the emotional experiences of others
- Social Coordination: Observing and controlling behavior to be involved in social situations
- Declarative language: The use of non-verbal communication and language to show curiosity, help interaction, share feelings and thoughts and coordinate actions with others
- Flexible Thinking: Adapt and change plans when situations change
- Relational Information Processing: Solve problems without clear solutions and solve situations that don’t have a “right or wrong” solution
- Foresight and Hindsight: Think about past experiences and foresee future possibilities in situations based on those past experiences
3. Sensory Integration Therapy
Sensory integration therapy is all about decreasing sensory sensitivities whether it be light, texture, noise, or touch. This therapy is mostly play-based and involves focusing on the things your child is most overly sensitive about. For example, if a child is overly sensitive to touch, a therapist will interact with the child by touching the back of his/her hand with different textures in hopes to desensitize him/her over time. Sensory integration is a form of occupational therapy and studies show it’s an effective intervention for those with autism ages four to 12.

Along with sensory integration therapy, your child may also need speech and language therapy. The main goal of speech therapy is a focus on communication and social interaction. Speech-language pathologists help a child communicate through the use of electronic talkers, sign language, picture boards, social skills development, pragmatic skills, sounds, and rhymes. These are all fundamental in helping a child increase verbal and non-verbal communication.
Floortime Play Therapy
Another form of therapy utilized by occupational and speech therapists is floortime play therapy. This type of therapy focuses on building into a child’s strengths by getting to their level of play. Instead of focusing on guiding a child through an activity, the child is the one leading all aspects of play.
Floortime play therapy is built upon six milestones:
- Self-regulation and interest in the world around them
- Emotional thinking
- Emotional ideas
- Back-and-forth communication
- Complex communication
- Intimacy and relationship engagement
To meet these milestones, a therapist or parent interacts with the child by following what the child is doing in a calm environment. If a child is playing with cars on the floor, a therapist or parent will sit on the floor and play with the cars. These play sessions normally last anywhere from two to five hours a day.

Over time, the interactions between the therapist and child become more complex. For instance, as a child plays with a toy car, toy planes are introduced with added language to create a game. Floortime play encourages your child to respond to questions and interact with the therapist.
In 2011, independent researchers in Thailand and Canada discovered floortime play therapy was “significantly improving emotional development and reducing autism’s core symptoms.”
Read more about Floortime Play Therapy
Recommended article
Floor time Play Therapy for Autism Kids
IEP Goals for Autism
Since the bulk of your child’s therapy will come from speech therapy, you may be curious about the goals of speech and language skills for a child on the autism spectrum. These same goals are not only for speech therapy but for your child’s IEP (Individualized Education Program). The following goals for IEP’s are only examples. Every child with autism requires different needs, therefore your child’s IEP goals will be specific to him/her.
Joint Attention
Joint attention refers to a child’s ability to focus on multiple things at once. This is essential when your child begins school. Your child needs to be able to focus on multiple tasks at once. While many children with autism struggle with joint attention, your child’s IEP can focus on specific areas of joint attention.
Here are some joint attention goals for your child’s IEP:
- Responding to the teacher’s voice
- Showing understanding through both eye contact and gestures
- Being able to recognize and describe the emotions of him/herself and others
Social Reciprocity
Social reciprocity is key for interacting with other people. It involves the back-and-forth interaction between two people. Children with autism spectrum disorder experience issues with social reciprocity like starting interaction, responding to interaction by others, maintaining conversations, and turn-taking verbal communication.
To help your child with social reciprocity, here are some goals for an IEP:
- Maintaining interactions
- Initiating conversations
- Engaging in topic maintenance
- Recognizing and attempting to repair communication breakdowns
Language and Related Cognitive Goals
Language is more than speaking. It’s understanding and using the native language with both verbal and nonverbal communication. Pointing, waving, and facial expressions are all examples of nonverbal communication.
Some examples of language and related cognitive goals for your child’s IEP can include:
- Using gestures
- Turning pages in a book while pointing at pictures
- Using words and gestures to share intentions
- Problem-solving
- Understanding event sequences (sequences in stories, alphabet letters)
- Using and combining words in creative combinations
Behavioral and Emotional Regulation
This area of a child’s IEP goals remains one of the hardest areas to master for children with autism. Behavioral and emotional regulation involves understanding emotions, processing emotions, communicating their feelings, and coping with difficult emotions.
Some examples for behavioral and emotional regulation goals for an IEP include:
- Asking for a soothing activity when upset
- Expressing emotions
- Talking through transitions in activities
- Perceiving and predicting social behavior in others to self-monitor behavior
Read more about IEP goals and autism
Recommended article
Speech and Language Goals for Autistic Kids
Video Modeling and Autism
Video modeling is another form of therapy recently introduced. But video modeling first appeared in 1982 by Steinborn and Knapp by using a combination of behavioral training with a classroom-based environment to teach traffic and pedestrian skills to children within the autism spectrum.
Today, video modeling is considered a go-to method for teaching social skills and helping speech delay with autism. The therapy is now advanced even further with the help of scientific studies about mirror neurons.

Mirror neurons are sensory-motor cells in the brain that trigger or activate when…
- An individual performs an action
- Sees another person perform the same action
These types of neurons are thought to be linked to social behaviors, especially empathy and imitation, possibly explaining social cognition in humans. To take advantage of mirror neurons video modeling for social skills is used for children with autism. Speech Blubs takes video modeling a step further by having children speak or model behaviors and skills. All your child has to do for video modeling is watch Speech Blubs videos and copy the word or action demonstrated by other children.
The Speech Blubs app and video modeling will give your child the following benefits:
- Confidence to perform copied tasks and speech in daily life
- Learn faster by seeing other children perform the behaviors
- Increase memory of learned behaviors through fun activities and games
Read more about the science behind mirror neurons, video modeling, and autism
Recommended article
Teaching Kids with Video Modeling
Autism and Speech
One speech disorder affecting 65% of children with autism is speech apraxia. Although there are many forms of apraxia, speech apraxia directly affects the tongue, lips, mouth, and jaw in producing clear speech sounds. On top of words sounding unclear, the same word may sound differently each time it’s spoken leading to inconsistent speech sounds. If a child shows signs of a communication disorder, it can be hard to distinguish whether the speech issue is due to apraxia or autism. Therefore, an evaluation from a speech-language pathologist should be conducted.
Some areas a speech-language pathologist will examine for diagnosing speech apraxia are:
- Errors with consonants and vowels – A child may say the same word different each time.
- Problems moving from sound to sound or syllable to syllable – This results in long pauses between words and troubles repeating a string of words.
- Unusual emphasis on certain parts of speech – A child may emphasize all the syllables of a word or sentence resulting in a “flat or robotic” tone of speech.

Other symptoms of apraxia of speech used for diagnosis include:
- Minimal babbling as a baby
- Troubles forming and saying long words
- Repeated attempts to pronounce a word
- Excessive use of nonverbal communication
- Removing consonants at the beginning or end of a word
- Problems making words
During an evaluation for speech apraxia, a speech pathologist will evaluate your child’s oral-motor strength and movements. This will be done by asking the child to smile, move his/her tongue, swallow, or lick a lollipop. The evaluation will also examine your child’s hearing, starting and responding to instructions, verbal and nonverbal communication skills.
To help you child with the skills above, here are 7 at-home speech activities to start today:
1. Model words with examples
Grab your child’s favorite toy and hold it next to your mouth and say the word of the toy clearly and slowly. This helps your child see your mouth movements.
2. Find ways to amplify or change your voice
This is a way to foster back and forth imitation. Use an empty paper towel roll or voice-change app to make different sounds.
3. Offer two items
While holding two objects near your mouth, clearly say the words of the objects and ask which item he/she would like. Once your child points or says a word to respond, repeat the word of the object again.
For example: “Would you like an apple or an orange?”
After your child points or says a word, repeat “You would like the orange.”

4. Add excitement to your words
Change the tone of your voice by emphasizing sound at the beginning and ends of words. This will keep your child’s attention and help with imitation.
5. Make sound effects
Add sound effects to books or while playing with toys during floortime play.
6. Repeat “core words” in simple sentences
Keep “core words” simple and your sentences short, while focusing on emphasizing the core words. If you’re blowing bubbles, try core words like “bubble” or “pop.”

7. Encourage imitation with songs
Use music to engage your child with imitating your mouth movements. Songs like “If You’re Happy and You Know It” and “Itsy Bitsy Spider.” Combine these songs with the actions and movements to go along with them.
Read more about apraxia and autism
Recommended article
Can Children on the Autism Spectrum have Apraxia of Speech?
ASD and Speech Delay
When a child has a speech delay, parents often wonder whether the speech delay is due to autism. Although a speech delay is a sign of autism, symptoms of a speech delay and autism are very different. If you suspect your child has a speech delay, it’s important to either diagnose or rule out autism as the cause of a speech delay.
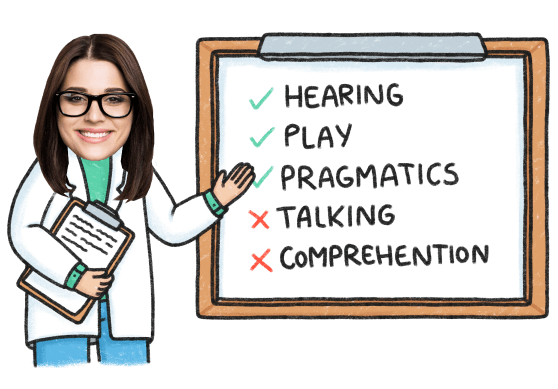
A speech-language pathologist can identify if your child is experiencing a speech delay but cannot diagnose autism. Only a developmental pediatrician can diagnose autism. To help you better understand the difference between speech delay and autism here are the signs and symptoms of both.

Signs and symptoms of autism:
- Delayed speech
- Lack of eye contact or brief eye contact
- Easily upset over minor changes in routine
- Reactions to certain sounds, lights, touch, smells, or tastes
- Difficulty understanding other’s emotions
- Focused on a small range of interests or objects
- Engages in repetitive behavior like spinning or rocking
- Does not respond to his/her name by 12 months
- Does not point at distant objects by 14 months
Signs and symptoms of a speech delay:
- Saying simple words clearly or unclearly by 12-15 months
- Not using nonverbal gestures like pointing and waving by 12 months
- Prefers to use gestures over words to communicate by 18 months
- Troubles imitating sound by 18 months
- Understanding simple words by 18 months
- Troubles understanding simple requests
- Only imitates speech or actions, but doesn’t produce words or phrases by 2 years
- Says some sounds or words repeatedly by 2 years
- Cannot use language to communicate needs by 2 years
- Cannot follow simple instructions by 2 years
- Unusual tone of voice (raspy/nasal sounding) by 2 years
- Talks in short sentences by 3 years
- Telling a story by 4-5 years
For more about speech delays read the article “If My Child Has Speech Delay Does That Mean They Have Autism?
Recommended article
If My Child Has a Speech Delay Do They Have Autism?
Nonverbal Autism
While it’s not an official diagnosis within the autism spectrum, nonverbal autism is used to describe any child that does not use verbal communication. Roughly 40% of children are considered nonverbal and there is no known cause of nonverbal autism. Societal misconceptions often associate nonverbal autism with low intelligence. However, nonverbal autism does not mean a lack of intelligence.
In 2015, Cambridge University found those with autistic traits are more likely to pursue careers in technology, engineering, science, and math. All of which require high intelligence. Another study holds promising results for future verbal communication for nonverbal children with autism.
Nonverbal autism is used to describe any child that does not use verbal communication.
The Center for Autism and Related Disorders studied records of children with autism between the ages of 8 to 17. All the participants’ experienced language delays of either being nonverbal or only speaking simple words or phrases.
The study found the following positive results:
- 70% of participants eventually spoke in simple sentences
- 47% of participants became fluent speakers
- Most participants had higher IQ’s then once thought
- Repetitive behaviors (rocking or spinning) and intense interests didn’t affect language development
Read more information about nonverbal autism
Recommended article
Will My Nonverbal Autistic Child Ever Talk?
Ways To Encourage Speech Development At Home
If your child has nonverbal autism, working with a speech-language pathologist is essential for increasing communication with your child. However, there are simple things you can do at home to strengthen your child’s speech development.
1. Focus on nonverbal communication
Add nonverbal communication by modeling it for your child. Increase eye contact. Nod or shake your head when saying yes or no. Point to objects you’re referring to. Learning these types of nonverbal cues increases communication of your child’s needs.

2. Shorten your speech
If your child struggles with following directions, it could be because of a short attention span and your directions are too long. Try focusing on “core words,” shortening phrases, and using simpler words. This will lessen confusion for your child.
Example: “Don’t stand on the chair!”
Shorten this phrase to: “Sit please.”
3. Imitate behavior
Play with your child by copy sounds or actions he/she does. Imitation is a vital part of development and research suspects it can predict language outcomes. The benefits of imitation include sharing emotions, understanding turn-taking, increasing attention, and helping a child take an interest in others socially.
Boost Your Child’s Speech Development!
Improve language & communication skills with fun learning!

4. Use visual tools
Many children with nonverbal autism require visual aids to help further understanding and communicate wants and needs. There are many apps like Speech Blubs that will help with speech development through imitation. A picture exchange communication system (PECS) is also essential for expressing needs and wants for a nonverbal child.
5. Encourage play and social interaction
Studies show children learn language best through play-based activities. Try singing songs, turn-taking activities, and gentle rough-housing. The most important part of play-based activities is being down at eye level with your child.

6. Leave “space” for your child to talk
Sometimes parents are too quick to answer for their child or they immediately ask a follow-up question. This may not leave enough “space” for your child to respond. Even if a nonverbal child responds with a gesture, it’s still communication. Over time, 15-20 seconds of space in between your questions can lead to an answer from your child.
7. Follow your child’s interests
It’s best to follow your child’s interests and focused attention on whatever he/she is doing. If your child is dumping out Legos on the floor, say “Dump Lego” and join in on the fun. This will help identify the action and increase language with short phrases and “core words.”
For more activities for nonverbal autism read 7 Ways To Help Your Child With Nonverbal Autism Speak
Recommended article
7 Ways to Help Your Child with Non-verbal Autism Speak
For a parents perspective for increasing speech for a child with nonverbal autism read 4 Ways To Help A Child With Nonverbal Autism Talk
Recommended article
4 Ways To Help A Child With Nonverbal Autism Talk
PECS And Autism
The Picture Exchange Communication System (PECS) is a way for nonverbal children to communicate without words. For children with autism and other developmental disabilities, PECS gives them a “voice” to communicate their needs and wants. Since the 1980s, PECS has been helping children and caregivers for short and long-term use for developing verbal speech.
Research found children understand pictures better after the age of three. Therefore, PECS is recommended for children three and older. Like any visual aid tool, the overall goal of PECS is the development of verbal speech. Some children progress through all six phases of the system and acquire verbal language. Other children continue to use this visual aid for communicating simple needs and wants.
PECS gives nonverbal children a “voice” to communicate their needs and wants.
For the PECS system to work correctly a child needs to be an “intentional” communicator. This means he/she displays a need to communicate needs. A child who is an “intentional” communicator may lead an adult by the hand to something he/she wants.
Here’s how the 6 phases of PECS work:
Phase 1: Learn how to communicate
This phase helps a child communicate his/her needs through pictures by using motivating factors like a favorite toy. For example: If your child loves trains, use a picture of a toy train to motivate him/her to exchange the picture for a train.
Phase 2: Learn persistence and picture distancing
Phase one builds upon phase two. A child will exchange pictures for a need, but picture distancing is also included. Picture distancing involves a child having to retrieve a card from far away to fulfill a need or want.
Phase 3: Making choices
This phase involves making choices. Two pictures are introduced, and a child needs to point or hand the card he/she chooses. This works best with motivating factors.

Phase 4: Express feelings and needs
This phase combines pictures and words to make short sentences. A child must combine “I want,” “I need,” or “I feel” cards with a picture of the desired object or feeling. Some children will only reach phase four in the PECS system.
Phase 5: Answering a question
Phase 5 builds upon phase 4 by using cards to answer questions. A child will combine a sentence card with a picture card to give the answer.
Phase 6: Comment on a question
Phase 6 involves elaborating upon phase 5 by commenting on questions.
How To Customize PECS For Your Child
Every child is different. Therefore, a PECS needs to be customized to meet your child’s unique needs, wants, likes, and dislikes. To customize PECS, you can either purchase premade picture cards or make your own. If you’re making your own, keep the following tips in mind!

Tips for customizing the PECS for your child:
- Focus on an area of need – These are pictures your child needs help with communicating the most. If your child needs help communicating he/she is hungry then focus on cards representing hunger. For example: Picture cards showing breakfast, lunch, and dinner foods, or your child’s favorite foods.
- Follow your child’s interests – A child will show more interest in PECS if there are cards with their favorite toys, foods, activities, and more.
- Cartoon versus real photo’s – PECS is either used with cartoon or real images. The best way to see how your child responds to one or the other is by creating some favorite images with both cartoon and real photo’s. Then see which one your child prefers to communicate with.
- Choose how to display PECS – How you choose to display PECS cards depends on the patience level of your child, his/her understanding, and if you choose to create a schedule with the cards. If you create a schedule, schedules will need to be displayed somewhere easily accessible.
Here are some other ways to display and store PECS cards:
- In a storage binder
- Laminated and held together by a keyring
- A schedule board with Velcro
- A communication book (this includes long Velcro strips to make sentences with picture cards)
For a parent’s perspective on customizing PECS read Customize A Picture Exchange Communication System For Your Child
Recommended article
Customize A Picture Exchange Communication System For Your Child
Stimming Behavior
Stimming behavior is a sign of autism. But individuals who do not have autism also engage in stimming behavior. Stimming behavior may occur in any who is anxious or nervous and takes the form of nail-biting, foot jiggling, knuckle cracking, and more. While some with autism may engage in these common stimming behaviors, stimming in children with autism looks different because he/she is unable to stop.
A child with autism may engage in the following stims:
- Rocking back-and-forth
- Hand flapping
- Bouncing
- Spinning
- Walking on tiptoes
- Repetitive blinking
- Rearranging or lining up objects
- Staring at ceiling fans or lights
- Sniffing people and objects
- Licking or rubbing objects
- Repeating words and phrases
It’s important to note a child can engage in one behavior or in multiple behaviors and each is done repetitively. While the list above are typical behaviors for children with autism, some children will display stims that cause physical harm.
Stimming behavior leading to physical harm include:
- Punching or biting
- Headbanging
- Excessive skin scratching
- Scab or sore picking
- Swallowing small objects
Although science is unsure what causes stimming in autism, there are multiple theories to this behavior:
- To stimulate or decrease the sensory system
- A way to adapt to an unfamiliar environment
- To calm him/herself
- Show frustration
- Avoid activities or expectations
While your child’s stimming may worry you, the behavior doesn’t need to be controlled unless it interferes with learning, causes social isolation, is dangerous or causes issues for other family members. If you are worried about the stimming behavior, there are simple ways to manage it.
How to manage stimming behavior:
- Sensory toys- Squeeze toys, sensory balls, moldable toys, fidget toys, etc.
- Eliminate medical conditions- Certain medical conditions like headaches, ear infections, and pain may be the cause or make stimming worse. Talk with your child’s doctor to ensure it’s not caused by other medical conditions.
- Provide a calm environment- Stimming becomes worse under stressful situations. Try to avoid situations where your child may be easily overwhelmed.
- Try exercise- Research shows physical activity releases tension to reduce stimming. It also provides stimulation for those needing it most.
- Teach self-regulation of emotions- This involves expressing emotions in a positive way compared to stimming, especially stimming behavior resulting in self-harm.
For more on stimming behavior read All About Stimming in Autism Kids
Recommended article
All about Stimming in Kids with Autism
For a parent’s perspective of stimming behavior read the article Stimming Behavior and Autism
Recommended article
Stimming Behavior and Autism: What it is, Causes And How To Manage It
Oral Stimming
Similar to common repetitive motion seen in children with autism, oral stimming involves taste-testing, chewing, and/or swallowing objects. Children who oral stim are often seen with clothing, toys, paper, sensory balls, pencils/pens, and other inanimate objects in their mouth.
But with oral stimming, there are potential dangers to watch out for.
- Small objects can be swallowed causing health issues
- Chewing on hard objects causes tooth damage
- Objects can cause chocking

If your child is a “chewer” there are ways to manage and remove potential chewing hazards.
- Inspect household objects frequently- Frequently check toys, books, and clothing for missing pieces or any signs of chewing.
- Offer chewy snacks- To provide a healthy outlet for oral sensory needs, offer chewy snacks like dry cereal, granola, popcorn, veggie chips, carrots, celery, apples, dried fruit, and fruit snacks.
- Try chewable jewelry- Bracelets, necklaces, and pencil toppers made specifically for children with oral sensory needs.
- Use redirection- If your child begins to chew on something he/she is not suppose to, redirect the chewing behavior to a “safe” object like sensory balls and chewable jewelry.
- Offer drinks with straws- Drinking through straws may fulfill the oral sensory need your child is craving.
For more on oral stimming read the article 5 Management Tips For Oral Stimming
Recommended article
5 Management Tips for Oral Stimming
Sensory Issues
Children with autism typically display signs of sensory processing disorder. Within sensory processing disorder, there are two times: Sensory avoider (hypersensitive) and sensory seeker (hyposensitive). Whether your child is a sensory seeker or sensory avoider, each type presents different symptoms. But children can display symptoms of both.
A child who is a sensory avoider struggles to process environmental stimuli and becomes easily overwhelmed, therefore they are overly sensitive to their environment. A sensory seeker is under-stimulated by his/her environment resulting in a child seeking out sensory stimulation.
Sensory avoider symptoms:
- Distracted by background noise (normally not noticeable to others)
- Avoids touch (hugs and cuddling)
- Appears clumsy (bumping into things)
- Doesn’t tolerate loud noises
- Becomes frightened easily by sudden loud noises
- Very particular about clothing
- Avoids crowds due to loud noise or the possibility of being touched
Sensory seeker symptoms:
- High pain tolerance
- Chews on inanimate objects (oral stimming)
- Stands too close to others
- Jumps, runs, and crashes into things
- Doesn’t understand his/her own strength
- Makes loud noises
- Stimming behavior (rocking, spinning)
- Explores the world through touch
Recommended article
Is Your Child A Sensory Seeker Or Avoider?
Synesthesia and Autism
Synesthesia is a rare condition affecting 1% percent of the population. It is a neurological condition where one sense is simultaneously perceived by one or more other senses. Although many people are born with the condition, it’s also possible to develop synesthesia later in life. Initial research indicates synesthesia may be genetically inherited.
People with synesthesia may…
- See the word “plane” as mint green
- Picture a skyscraper, but taste blueberries
- Read the number two, but see red
While there’s no specific way to diagnose synesthesia, Richard Cytowic, MD and leading synesthesia researcher created specific guidelines for doctors to determine if a child has synesthesia.
Synesthesia guidelines for diagnosis:
- Involuntary – Perceptions are not actively thought about, they just happen.
- Projected – Instead of seeing things like a color in the “mind’s eye,” a person will see the color outside their body.
- Durable and generic – The perceptions must be consistent each time. For instance, when someone hears a particular song, he/she tastes chocolate.
- Memorable – The synesthetic perception is remembered over the primary perception. For example, if someone associates the name “Laura” with the color purple, he/she will remember purple and not “Laura.”
Research is now pointing to a connection between autism and synesthesia. Individuals with autism and synesthesia report higher levels of sensory sensitivity. Further research also reports synesthesia tends to appear in individuals with autism who have abilities in memory, art, arithmetic as well as high intelligence.
Although synesthesia doesn’t present any problems for a child, if you suspect your child may have synesthesia it’s important to get he/she diagnosed to better understand how your child views the world along with autism.
For more information about this condition, read the article Is There A Link Between Synesthesia And Autism?
Recommended article
Is There a Link between Synesthesia and Autism?
Food Aversions and Autism
Picky eating is common among children. But for children with autism picky eating turns into food aversions. Research studies found children with autism are five times more likely to have fewer food selections, more mealtime tantrums, and ritualistic eating. Autism Parenting Magazine reports children with autism often limit food options to less than five types.

While the specific cause of food aversion and autism is unknown, it’s suspected that sensory issues related to food are to blame. Bright colored food may lead to sensory overload causing specific foods like peppers to be avoided altogether. The texture of certain foods may also lead to an aversion. For instance, a child may avoid pasta because he/she dislikes the feel of wet noodles.
Food aversions are challenging for parents with an autistic child. Although your child may be extremely picky about his/her food choices, there are things you can do to help expose your child to new foods to increase food selection.
5 Tips for introducing new food
1. Don’t pressure
Don’t try and convince your child to “clear their plate.” This will only lead to further food aversions. Instead, each time a new food item is introduced, simply leave it on the plate and allow your child to decide to eat it or not.
2. Don’t intermix foods
Foods that are intermixed may lead to sensory overload. That sensory overload will only result in food aversions and mealtime tantrums. To avoid this, keep each food item separate. For instance, if you have pasta with broccoli, cheese, and chicken, separate each ingredient. Don’t try and ‘hide’ food ingredients in hopes your child won’t notice.
3. Combine new and old favorites
Always combine a new food item with one of your child’s favorite foods. If you would like to introduce green beans, pair it with his/her favorite like chicken nuggets. This will give your child the choice to eat the green beans or not while ensuring he/she eat something during mealtime.
4. Eat the same new food
Children with autism learn best through visualization. Show your child the new food item is tasty by eating it yourself. Over time, your child will see the new food item being eaten over and over and may start eating it themselves.
5. Allow them to explore
Instead of keeping your child from playing with his/her food, encourage it! For children with sensory issues, play is key for introducing new foods. Allow your child to taste, smell, and feel the food to get use to it.
Read more about food aversions and autism
Recommended article
Autism and Food Aversions: 5 Tips for Introducing New Food
Resources, Books and Magazines on Autism for Parents
Autism Parenting Magazine
The prime resource for parents of kids with autism, Autism Parenting Magazine, recently included us in their Helpful Links section! To be endorsed by this noted authority on how to survive and thrive as parents of kids on the Autism Spectrum is an honor, indeed. For even more information about where to find resources for dealing with this challenging disorder, also see Autism Resources for Parents – The Ultimate New Guide.
FREE professional PECS cards and images
Professional, printable and customizable PECS cards.
National Autism Resources
Find resources for sensory items and classroom.
Autism Speaks
Leading authority on all information related to autism.
Conclusion
Autism spectrum disorder is a complicated diagnosis. There’s no specific cause to its existence and each child displays very different symptoms and severities. This makes it challenging for parenting a child with autism.
Children with autism need extra time to develop at their own rate with the help of doctors, therapy, tools, and a loving and patient parent like yourself! If you believe your child may have autism, an early diagnosis is key. The earlier the signs and symptoms of autism are recognized and diagnosed, the sooner your child will receive the necessary therapy to flourish and reach his/her full potential!